Mental Health & The Tales We Tell Ourselves: Part 3
Is the mental health “epidemic” due to personal failings, or is it a systemic issue?
Escrito por Conor Truax
01 This is part three of a four part series exploring mental health, from the language we use to social media to the role of labels play on our identity.
02 People often speak about mental health as an individual, medicalized issue that can be cured or self-optimized.
03 Conor proposes that mental health is nuanced, reactive to our environment, and something we work on for the rest of our lives.
Headlines today often speak of “the mental health epidemic” in the context of individual suffering: a singular overdose, a suicide, a crime. We reduce larger collective struggles to tragic personal cases, and then pay no mind to why these tragedies happened in the first place.
In his book, Madness and Civilization, Michel Foucault describes madness as “the false punishment of a false solution, that by its own virtue brings light to the real problem which can then be truly resolved.” In other words, population-level increases in mental illness are a symptom of failings in our society, rather than a cause in and of itself. It seems we continually fail to investigate and correct these failings that have led to our “mental health epidemic”.
In the New York Times, Danielle Carr explains that the medicalization of mental health does not work to solve the underlying cause of population-wide increases in mental illness — all it does is reduce a complicated social problem to a simple, actionable cause.
Here’s an example: The reductive and now infamous chemical-imbalance model that argues depression and other mental illnesses are caused by neurotransmitter imbalance (similar to an equilibrium math problem that simply needs to be solved). Despite consensus among many clinicians that the model was reductive, the idea still spread within pop culture. This led to the promotion of SSRI use, without any attention on other important factors, such as integrated uses of therapy and community building.
This example of simplified medicalization manifests itself in the broader trend of the “mental health epidemic” — the language itself representing internal, mental health experiences as something that can be caught and spread from individual to individual, and solved by immunization or linear care.
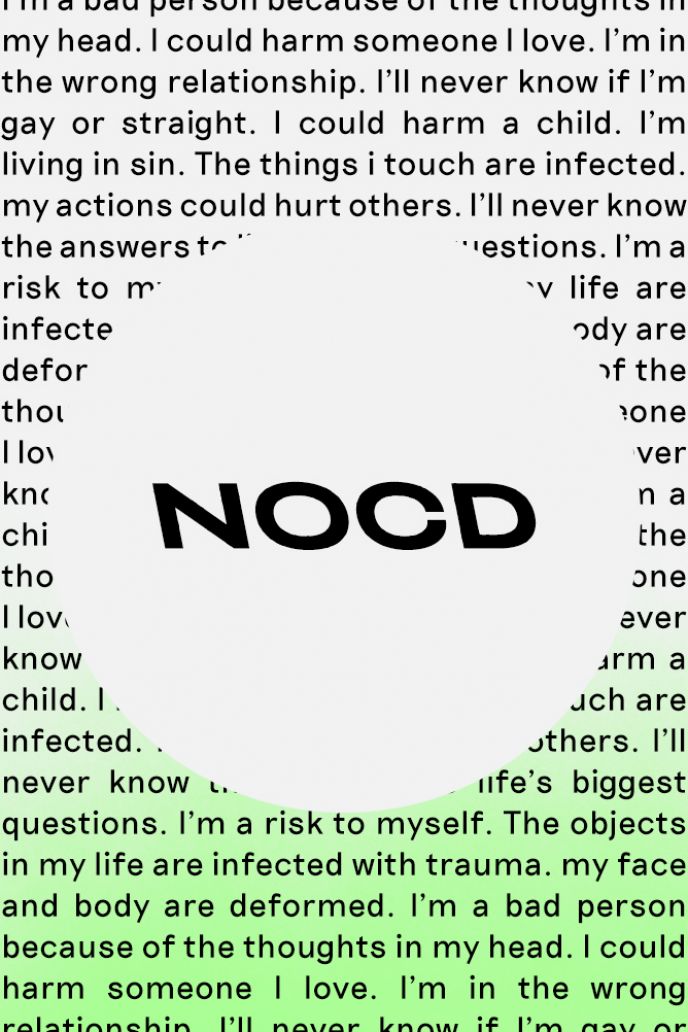
When my symptoms of OCD became apparent during the pandemic, it was my mental health’s reaction to an existential crisis at play, rather than an existential crisis alone. But at the time, I was convinced that what I was experiencing was unique to me alone. I was surprised to discover that I could relate to fellow sufferers online, most of whom were in the deepest throes of their difficulties.
Condiciones relacionadas
I succumbed to a practice that we all do to some degree: rather than viewing mental health as reactive to the world at large, we instead individualize suffering. Whether with pity or impatience, this causes us to treat sufferers as victims, which only contributes to the narratives of despair we continue to tell ourselves. Beyond frequent misuse, phrases like “I’m so OCD,” “He’s bipolar,” and “We’re depressed” reduce mental illness to forms of identity, rather than experiences we can actionably address.
Mental health management is a lifelong journey for everyone. Reducing suffering to a diagnostic binary rather than spectra that everyone falls along only serves to isolate, and embed this false narrative into identity.
*
Much of our lives are lived online, which means that when we begin asking ourselves questions like, “Where can I get help?” rarely do we first turn to a doctor or mental healthcare professional. We ask Google.
Unfortunately, the internet is full of savvy marketers who want to catch our attention with how they can “cure” our “negative” experiences by “hacking” our brains and bodies. These ventures paint the human experience as a problem to be solved, should we choose to commit ourselves to their wellness activities. Yet again, we find ourselves following a linear path of recovery.
There’s a fundamental Buddhist teaching that says that you cannot pursue meditation in a rigid search for enlightenment — you need to commit yourself to the practice whether or not enlightenment ever comes.
But today we are literate only in the reward, the end, the resolution. This has only gotten worse with social media. Yes, we post on LinkedIn and Instagram, but we also share our fitness activities on Strava and set meditation streaks on Headspace. The thing is, none of these metrics capture what any of these activities do for us physically, spiritually, or emotionally.
You could go to the gym five days per week and feel unfulfilled. Or you could go twice per week and reap greater joy from fewer, more focused sessions. I found myself in the trap of the former for too long, evidenced by my laundry list of half-attempted diets and cursory meditations. I’ll tell you a secret: nothing helped until I stopped fixating on whether it did or it didn’t.
By striving toward self-optimization — a constant happy state — we put ourselves at odds with the full range of human emotions. Worse, this culture leads us to fixate on what is “negative” or “wrong” with us, trapping us in a cycle of overpathologizing and self-problematization.
As we step away from this thinking, another Buddhist phrase comes to mind: “There is no path to happiness. Happiness is the path.” Happiness is an emotion that comes and goes, and resistance to this changing state will only result in friction. Be mindful of that path, and its edges. There is no end.
<>
This is part three of a four part essay.
Click here for Part One
Click here for Part Two
Click here for Part Four
You can find Conor here.
Apoya nuestro trabajo
Nuestra misión es cambiar la manera en que el mundo percibe la salud mental.